KDIGO Clinical Practice Guideline for Acute Kidney Injury
Introduction and Methodology
AKI Definition
Prevention and Treatment of AKI
Contrast-induced AKI
Dialysis Interventions for Treatment of AKI
Organization and Acknowledgements
Section 3: Prevention and Treatment of AKI
- 3.1.1: In the absence of hemorrhagic shock, we suggest using isotonic crystalloids rather than colloids (albumin or starches) as initial management for expansion of intravascular volume in patients at risk for AKI or with AKI. (2B)
- 3.1.2: We recommend the use of vasopressors in conjunction with fluids in patients with vasomotor shock with, or at risk for, AKI. (1C)
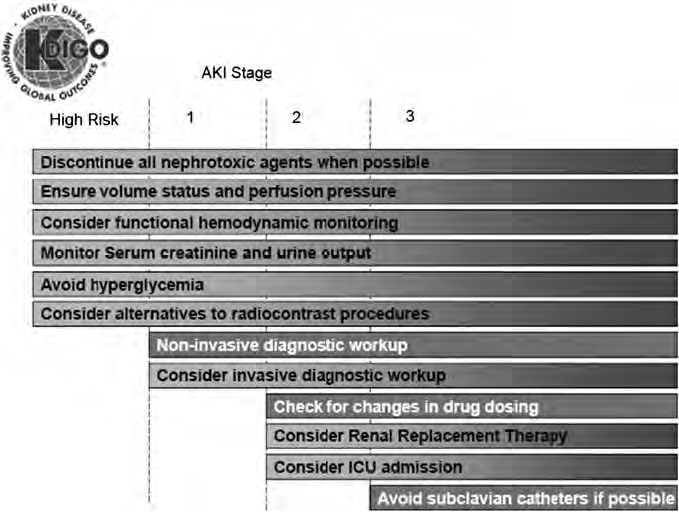
Figure 4 | Stage-based management of AKI. Shading of boxes indicates priority of action—solid shading indicates actions that are equally appropriate at all stages whereas graded shading indicates increasing priority as intensity increases. AKI, acute kidney injury; ICU, intensivecare unit.
- 3.1.3: We suggest using protocol-based management of hemodynamic and oxygenation parameters to prevent development or worsening of AKI in high-risk patients in the perioperative setting (2C) or in patients with septic shock (2C).
- 3.3.1: In critically ill patients, we suggest insulin therapy targeting plasma glucose 110–149mg/dl (6.1–8.3mmol/l). (2C)
- 3.3.2: We suggest achieving a total energy intake of 20–30 kcal/kg/d in patients with any stage of AKI. (2C)
- 3.3.3: We suggest to avoid restriction of protein intake with the aim of preventing or delaying initiation of RRT. (2D)
- 3.3.4: We suggest administering 0.8–1.0 g/kg/d of protein in noncatabolic AKI patients without need for dialysis (2D), 1.0–1.5 g/kg/d in patients with AKI on RRT (2D), and up to a maximum of 1.7 g/kg/d in patients on continuous renal replacement therapy (CRRT) and in hypercatabolic patients. (2D)
- 3.3.5: We suggest providing nutrition preferentially via the enteral route in patients with AKI. (2C)
- 3.4.1: We recommend not using diuretics to prevent AKI. (1B)
- 3.4.2: We suggest not using diuretics to treat AKI, except in the management of volume overload. (2C)
- 3.5.1: We recommend not using low-dose dopamine to prevent or treat AKI. (1A)
- 3.5.2: We suggest not using fenoldopam to prevent or treat AKI. (2C)
- 3.5.3: We suggest not using atrial natriuretic peptide (ANP) to prevent (2C) or treat (2B) AKI.
- 3.6.1: We recommend not using recombinant human (rh)IGF-1 to prevent or treat AKI. (1B)
- 3.7.1: We suggest that a single dose of theophylline may be given in neonates with severe perinatal asphyxia, who are at high risk of AKI. (2B)
- 3.8.1: We suggest not using aminoglycosides for the treatment of infections unless no suitable, less nephrotoxic, therapeutic alternatives are available. (2A)
- 3.8.2: We suggest that, in patients with normal kidney function in steady state, aminoglycosides are administered as a single dose daily rather than multiple-dose daily treatment regimens. (2B)
- 3.8.3: We recommend monitoring aminoglycoside drug levels when treatment with multiple daily dosing is used for more than 24 hours. (1A)
- 3.8.4: We suggest monitoring aminoglycoside drug levels when treatment with single-daily dosing is used for more than 48 hours. (2C)
- 3.8.5: We suggest using topical or local applications of aminoglycosides (e.g., respiratory aerosols, instilled antibiotic beads), rather than i.v. application, when feasible and suitable. (2B)
- 3.8.6: We suggest using lipid formulations of amphotericin B rather than conventional formulations of amphotericin B. (2A)
- 3.8.7: In the treatment of systemic mycoses or parasitic infections, we recommend using azole antifungal agents and/or the echinocandins rather than conventional amphotericin B, if equal therapeutic efficacy can be assumed. (1A)
- 3.9.1: We suggest that off-pump coronary artery bypass graft surgery not be selected solely for the purpose of reducing perioperative AKI or need for RRT. (2C)
- 3.9.2: We suggest not using NAC to prevent AKI in critically ill patients with hypotension. (2D)
- 3.9.3: We recommend not using oral or i.v. NAC for prevention of postsurgical AKI. (1A)
By using this site you acknowledge that you have read, understand, and agree to be bound by our terms of use and privacy policy. All content and tools are for educational use only, are not meant to be a substitute for professional advice and should not be used for medical diagnosis and/or medical treatment.