KDIGO Clinical Practice Guideline for Acute Kidney Injury
Introduction and Methodology
AKI Definition
Prevention and Treatment of AKI
Contrast-induced AKI
Dialysis Interventions for Treatment of AKI
Organization and Acknowledgements
Section 5: Dialysis Interventions for Treatment of AKI
- 5.1.1: Initiate RRT emergently when life-threatening changes in fluid, electrolyte, and acid-base balance exist. (Not Graded)
- 5.1.2: Consider the broader clinical context, the presence of conditions that can be modified with RRT, and trends of laboratory tests—rather than single BUN and creatinine thresholds alone—when making the decision to start RRT. (Not Graded)
- 5.2.1: Discontinue RRTwhen it is no longer required, either because intrinsic kidney function has recovered to the point that it is adequate to meet patient needs, or because RRT is no longer consistent with the goals of care. (Not Graded)
- 5.2.2: We suggest not using diuretics to enhance kidney function recovery, or to reduce the duration or frequency of RRT. (2B)
- 5.3.1: In a patient with AKI requiring RRT, base the decision to use anticoagulation for RRT on assessment of the patient’s potential risks and benefits from anticoagulation (see Figure 17). (Not Graded)
- 5.3.1.1: We recommend using anticoagulation during RRT in AKI if a patient does not have an increased bleeding risk or impaired coagulation and is not already receiving systemic anticoagulation. (1B)
- 5.3.2: For patients without an increased bleeding risk or impaired coagulation and not already receiving effective systemic anticoagulation, we suggest the following:
- 5.3.2.1: For anticoagulation in intermittent RRT, we recommend using either unfractionated or low-molecularweight heparin, rather than other anticoagulants. (1C)
- 5.3.2.2: For anticoagulation in CRRT, we suggest using regional citrate anticoagulation rather than heparin in patients who do not have contraindications for citrate. (2B)
- 5.3.2.3: For anticoagulation during CRRT in patients who have contraindications for citrate, we suggest using either unfractionated or low-molecular-weight heparin, rather than other anticoagulants. (2C)
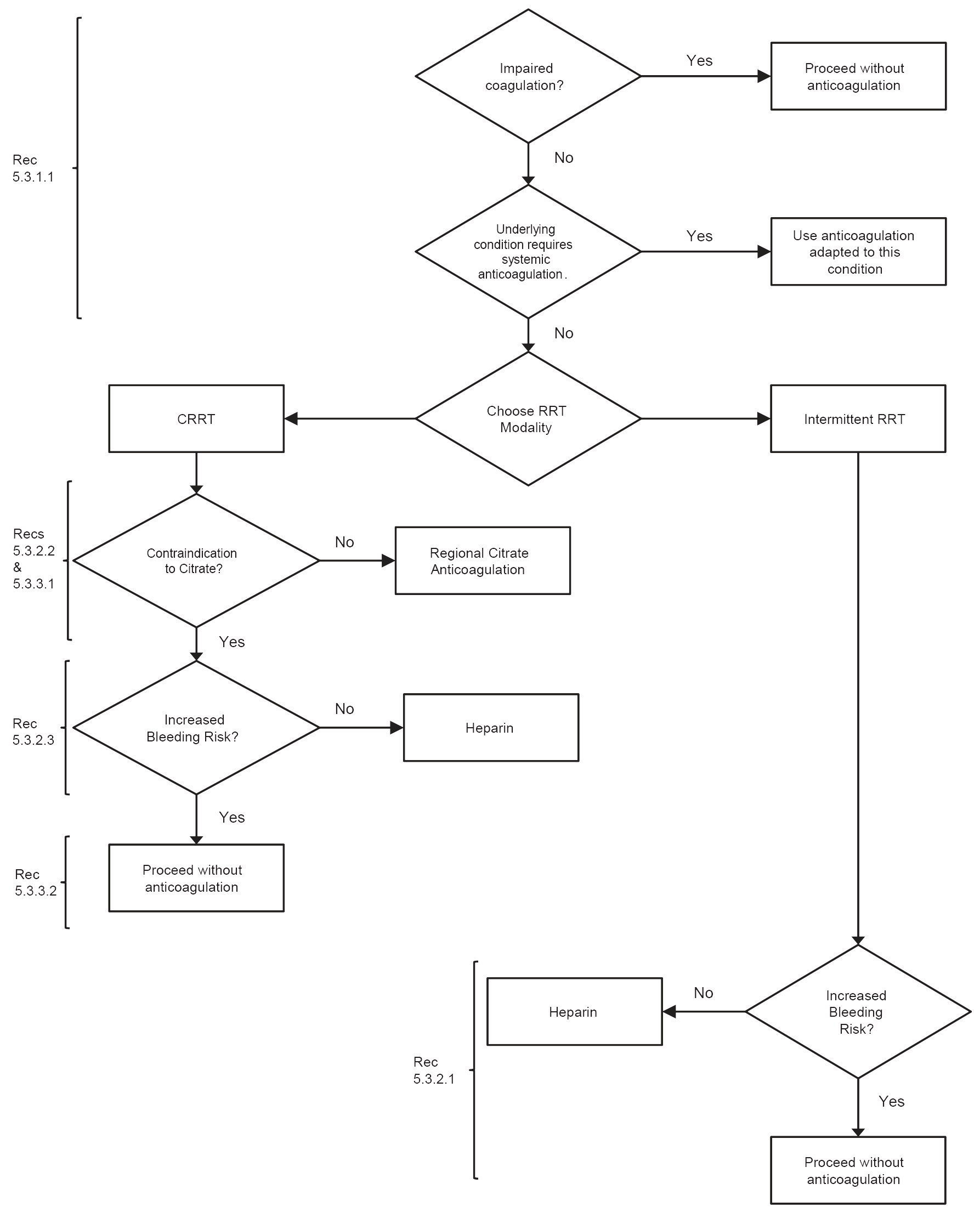
Figure 17 | Flow-chart summary of recommendations. Heparin includes low-molecular-weight or unfractionated heparin. CRRT, continuous renal replacement therapy; RRT, renal replacement therapy.
- 5.3.3: For patients with increased bleeding risk who are not receiving anticoagulation, we suggest the following for anticoagulation during RRT:
- 5.3.3.1: We suggest using regional citrate anticoagulation, rather than no anticoagulation, during CRRT in a patient without contraindications for citrate. (2C)
- 5.3.3.2: We suggest avoiding regional heparinization during CRRT in a patient with increased risk of bleeding. (2C)
- 5.3.4: In a patient with heparin-induced thrombocytopenia (HIT), all heparin must be stopped and we recommend using direct thrombin inhibitors (such as argatroban) or Factor Xa inhibitors (such as danaparoid or fondaparinux) rather than other or no anticoagulation during RRT. (1A)
- 5.3.4.1: In a patient with HIT who does not have severe liver failure, we suggest using argatroban rather than other thrombin or Factor Xa inhibitors during RRT. (2C)
- 5.4.1: We suggest initiating RRT in patients with AKI via an uncuffed nontunneled dialysis catheter, rather than a tunneled catheter. (2D)
-
5.4.2:
When choosing a vein for insertion of a dialysis catheter in patients with AKI, consider these preferences (Not Graded):
- First choice: right jugular vein;
- Second choice: femoral vein;
- Third choice: left jugular vein;
- Last choice: subclavian vein with preference for the dominant side.
- 5.4.3: We recommend using ultrasound guidance for dialysis catheter insertion. (1A)
- 5.4.4: We recommend obtaining a chest radiograph promptly after placement and before first use of an internal jugular or subclavian dialysis catheter. (1B)
- 5.4.5: We suggest not using topical antibiotics over the skin insertion site of a nontunneled dialysis catheter in ICU patients with AKI requiring RRT. (2C)
- 5.4.6: We suggest not using antibiotic locks for prevention of catheter-related infections of nontunneled dialysis catheters in AKI requiring RRT. (2C)
- 5.5.1: We suggest to use dialyzers with a biocompatible membrane for IHD and CRRT in patients with AKI. (2C)
- 5.6.1: Use continuous and intermittent RRT as complementary therapies in AKI patients. (Not Graded)
- 5.6.2: We suggest using CRRT, rather than standard intermittent RRT, for hemodynamically unstable patients. (2B)
- 5.6.3: We suggest using CRRT, rather than intermittent RRT, for AKI patients with acute brain injury or other causes of increased intracranial pressure or generalized brain edema. (2B)
- 5.7.1: We suggest using bicarbonate, rather than lactate, as a buffer in dialysate and replacement fluid for RRT in patients with AKI. (2C)
- 5.7.2: We recommend using bicarbonate, rather than lactate, as a buffer in dialysate and replacement fluid for RRT in patients with AKI and circulatory shock. (1B)
- 5.7.3: We suggest using bicarbonate, rather than lactate, as a buffer in dialysate and replacement fluid for RRT in patients with AKI and liver failure and/or lactic acidemia. (2B)
- 5.7.4: We recommend that dialysis fluids and replacement fluids in patients with AKI, at a minimum, comply with American Association of Medical Instrumentation (AAMI) standards regarding contamination with bacteria and endotoxins. (1B)
- 5.8.1: The dose of RRT to be delivered should be prescribed before starting each session of RRT. (Not Graded) We recommend frequent assessment of the actual delivered dose in order to adjust the prescription. (1B)
- 5.8.2: Provide RRT to achieve the goals of electrolyte, acid-base, solute, and fluid balance that will meet the patient’s needs. (Not Graded)
- 5.8.3: We recommend delivering a Kt/V of 3.9 per week when using intermittent or extended RRT in AKI. (1A)
- 5.8.4: We recommend delivering an effluent volume of 20–25 ml/kg/h for CRRT in AKI (1A). This will usually require a higher prescription of effluent volume. (Not Graded)
By using this site you acknowledge that you have read, understand, and agree to be bound by our terms of use and privacy policy. All content and tools are for educational use only, are not meant to be a substitute for professional advice and should not be used for medical diagnosis and/or medical treatment.